How to treat sleep apnea
If you are diagnosed with sleep apnea, your doctor may make recommendations to help you maintain an open airway during sleep. For those who are diagnosed with mild to moderate sleep apnea, you may be able to use a nighttime mouthpiece to prevent airway obstruction. This mouthpiece is called a mandibular advancement device or MAD.
A MAD can help many people without the need of a machine blowing air down into your lungs like a CPAP. If your doctor thinks that a MAD will be the right treatment, you can avoid the recurring costs and annoyances of a CPAP machine. In fact, most people who have tried a CPAP cannot sleep with it on or do not use it correctly, or every night as directed. If you are not using it, then it is not helping.
A MAD can even help a severe sleep apnea patient have better rest if they have tried a CPAP and just cannot wear it due to comfort reasons.
MAD Device (Mandibular Advancement Device)
To be used as an alternative to CPAP, a MAD is worn only during sleep, an oral appliance fits like a sports mouth guard or an orthodontic retainer. It supports the jaw in a forward position to help maintain an open upper airway. Research shows that oral appliance therapy is an effective treatment option for snoring and obstructive sleep apnea.
Why It Is Different From CPAP?
- Noninvasive
- Reimbursable through insurance
- Mostly effective for mild to moderate sleep apnea and snoring
- Requires no electricity and is portable enough for easy travel
- Noiseless
- Easy to clean
- Therapy is easy to wear and considered more comfortable than CPAP, which means patients are more likely to comply with therapy all the time
- Use also improves daytime sleepiness, driving performance, blood pressure, and quality of life
- Quick adjustment period for the user
Who is Affected by Sleep Apnea?
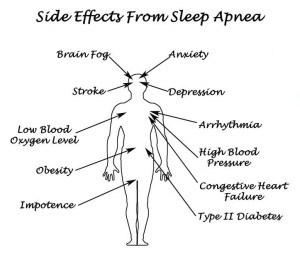
Anyone can suffer from sleep apnea. It can be caused by a person’s physical structure or medical conditions. These include obesity (obesity is a common cause of sleep apnea in adults. People with this condition have increased fat deposits in their necks that can block the upper airway). Large tonsils, endocrine disorders, neuromuscular disorders,heart or kidney failure, certain genetic syndromes, and premature birth.
What is Sleep Apnea?
Sleep apnea is a common condition in the United States. It can occur when the upper airway becomes blocked repeatedly during sleep, reducing or completely stopping airflow. This is known as obstructive sleep apnea. If the brain does not send the signals needed to breathe, the condition may be called central sleep apnea.
Common Signs of Sleep Apnea:
- Reduced or absent breathing, known as apnea events
- Frequent loud snoring
- Gasping for air during sleep
Common Symptoms of Sleep Apnea:
- Excessive daytime sleepiness and fatigue
- Decreases in attention, vigilance, concentration, motor skills, and verbal and visuospatial memory
- Dry mouth or headaches when waking
- Sexual dysfunction or decreased libido
- Waking up often during the night to urinate
How to Diagnose Sleep Apnea:
To screen for sleep apnea or other sleep disorders, your doctor may ask you about common signs and symptoms of this condition, such as how sleepy you feel during the day or when driving, and whether you or your partner has noticed that you snore, stop breathing, or gasp during your sleep. Your doctor may ask questions to assess your risk for developing this condition and take your physical measurements. Your doctor will also want to see whether you have any complications of undiagnosed sleep apnea, such as high blood pressure that is difficult to control.
If the screening suggests a sleep breathing disorder, we offer a take home sleep apnea screening device called an IPat. This machine will monitor your vitals while you sleep and record things like Light, Deep, and REM sleep, oxygen levels, apnea events (how many times you stop breathing), which side you sleep better on and decibels of snoring.